
Medical record-keeping in claims
Summary: What are the main issues raised in member claims in relation to record-keeping? Find out the underlying themes across all specialties and insights to reduce your risk of these types of claims, in our analysis.
Wednesday, 1 July 2020
Key learnings
- Medical records should convey enough information to ensure safe and effective ongoing care of the patient.
- Wherever practical, document your clinical reasoning: why you reached a certain diagnosis, performed a test, or prescribed a drug and any significant negative history or examinations.
Poor record-keeping was frequently associated with an inadequate standard of care
- Record-keeping issues were rarely the main reason for the claim (\ 1% of matters). They usually arose in addition to problems with other aspects of care.
- Poor record-keeping was much more commonly identified in claims where the doctor’s care was considered below standard on the main issue, than those where it met standard.
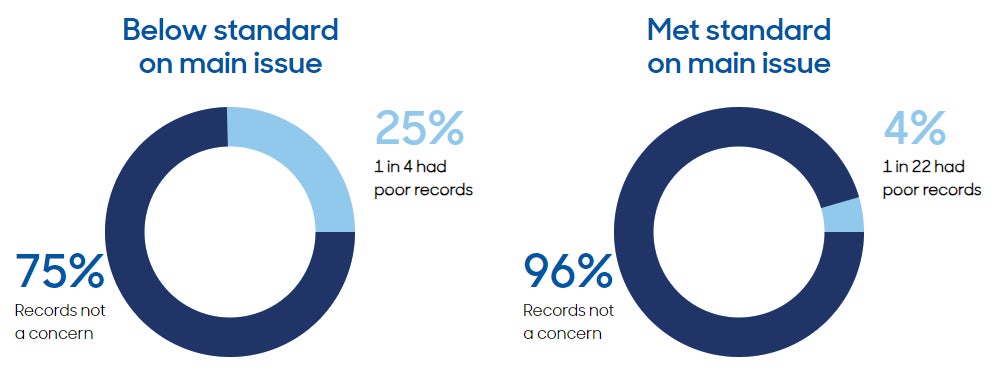
Note: The above does not show claims where standard of care on main issue is unknown, this occurs when the standard was not assessed, or the final assessment report was unavailable.
Good record-keeping makes claims easier to defend
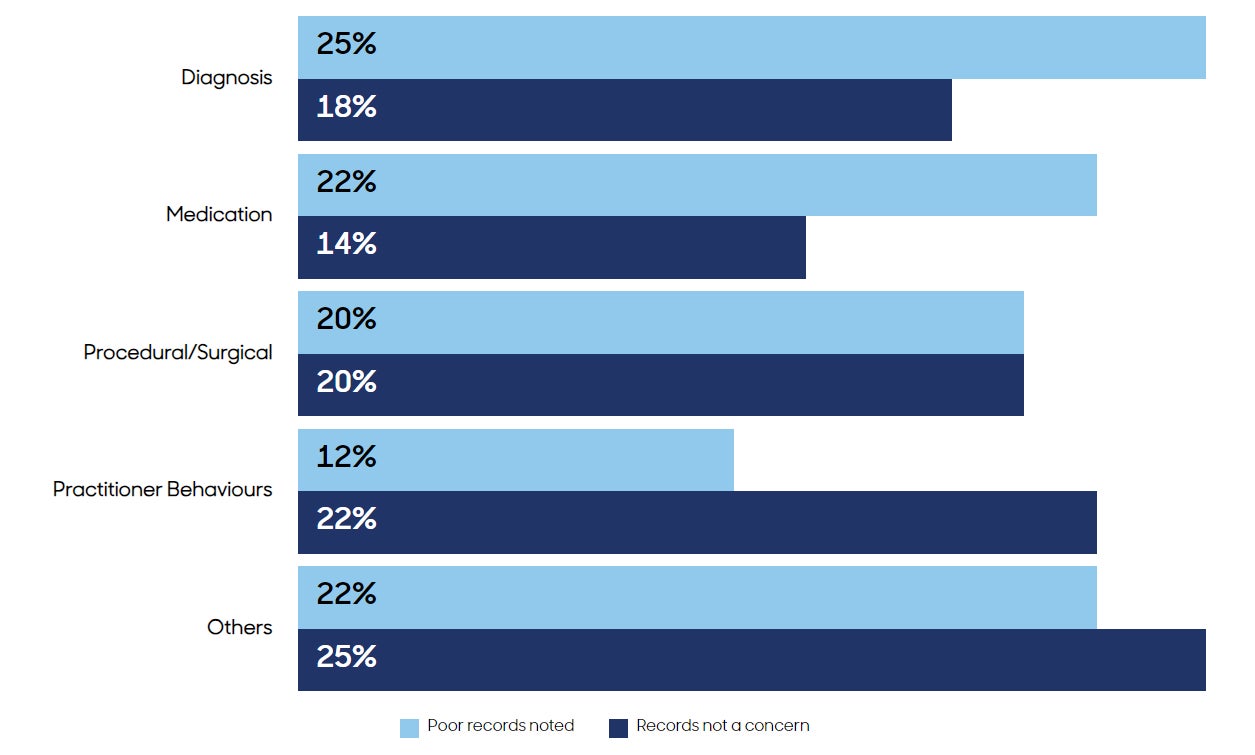
- Poor record-keeping most commonly arose in claims related to diagnosis, followed by claims related to medication.
- Inadequate records can affect claim outcomes, e.g. claims that could not be defended because of incomplete or missing records.
- Complaints to regulators resulted in more severe outcomes when records were found to be poor.
Records should document important details of patient care, within real-world constraints
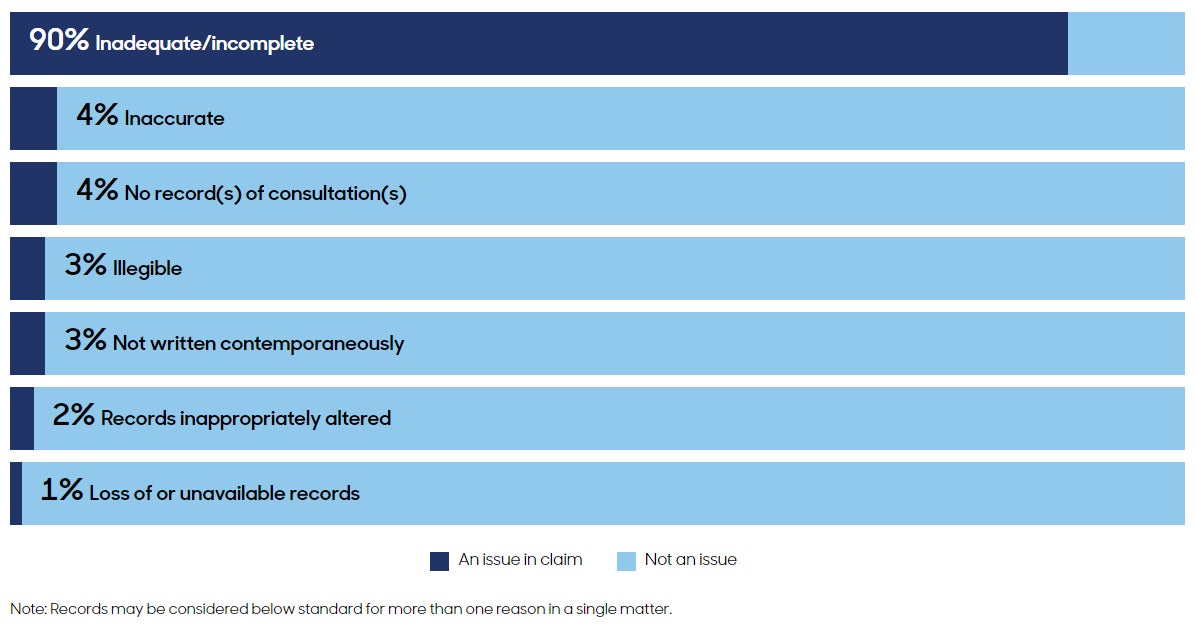
- Records considered below standard were almost always inadequate or incomplete. For example:
- not documenting important verbal discussions about risks of complications or treatment options
- omitting details about physical examinations, tests or treatments performed
- not documenting negative history or findings, and diagnosis considered but ruled out.
- Records should convey enough information to ensure safe and effective ongoing care of the patient, and document clinical reasoning.
- If records cannot be completed at the time of the consultation they should be updated as soon as possible afterwards. Document both the time of the consultation and the time the record was made.
More about this analysis
This report is based on our analysis of the underlying themes in 8,374 complaints to regulators and compensation claims for practising Avant members from all medical specialties, finalised between July 2016 and June 2019.
The report focuses on claims and complaints where record-keeping was the main issue or a contributing factor, or an additional area of concern identified during a medico-legal evaluation. The evaluation is undertaken following a claim to assess whether the expected standards of care were met. Claims involving poor record-keeping were classified as those for which the doctor’s record-keeping was assessed as being below expected standards.
For any queries, please contact us at research@avant.org.au
Member resources
For articles, factsheets, case studies and other resources on a range of topics, including documentation and medical records, visit the Avant Learning Centre.
Disclaimers
IMPORTANT: Avant routinely codes information collected in the course of assisting member doctors in medico-legal matters into a standardised, deidentified dataset. This retrospective analysis was conducted using this dataset. The findings represent the experience of these doctors in the period of time specified, which may not reflect the experience of all doctors in Australia. This publication is not comprehensive and does not constitute legal or medical advice. You should seek legal or other professional advice before relying on any content, and practise proper clinical decision-making with regard to the individual circumstances. Persons implementing any recommendations contained in this publication must exercise their own independent skill or judgement or seek appropriate professional advice relevant to their own particular practice. Compliance with any recommendations will not in any way guarantee discharge of the duty of care owed to patients and others coming into contact with the health professional or practice. Avant is not responsible to you or anyone else for any loss suffered in connection with the use of this information. Information is only current at the date initially published (June 2020). © Avant Mutual Group Limited 2020.