
Medical record issues in claims
What are the main issues raised in member claims in relation to medical records. Find out the underlying themes across all specialties and insights to reduce your risk of these types of claims, in our analysis.
Monday, 24 February 2025
Overview | Practice points |
|
|
All data is based on Avant claims and complaints closed from 1 July 2019 to 30 July 2024.
Medical record issues identified in 1 out of 5 claims
In the majority of claims where medical records were identified as an issue, records were found to be inadequate or incomplete. For example:
- not documenting important verbal discussions about risks of complications or treatment options
- omitting details about physical examinations, tests or treatments performed
- not documenting negative history or findings, and diagnosis considered but ruled out.
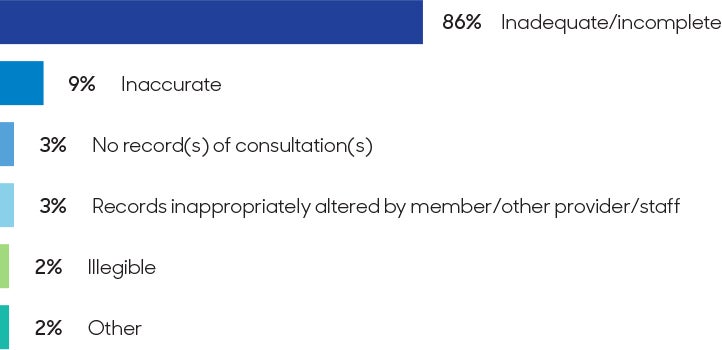
(Each claim may have more than one allegation about medical records.)
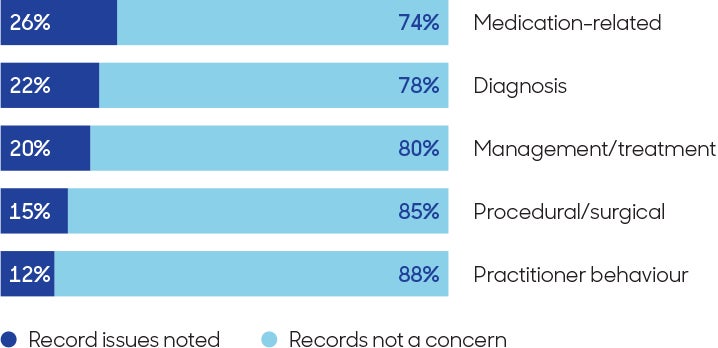
Medical record issues are often identified in claims about medication and diagnosis
- Most of the medication-related claims identified involved prescribing drugs of dependence.
- The diagnosis-related claims identified primarily concerned the initial assessment stage, with inadequate examination and failure to refer for diagnostic testing among the allegations.
Poor medical records can compromise the outcome of a claim
- Our analysis indicates a significant relationship between the quality of medical records and the outcome of a claim. Those with poor records were more likely to be assessed as below standard on the main issue than claims with good records.*
- Claims could not be defended in some cases due to incomplete or missing records.
- Complaints to regulators resulted in more severe outcomes when records were found to be poor.
*Statistically significant relationship between the two variables based on chi-square test of independence, X2 (1, N=14205) =1051.78, p is less than .01.
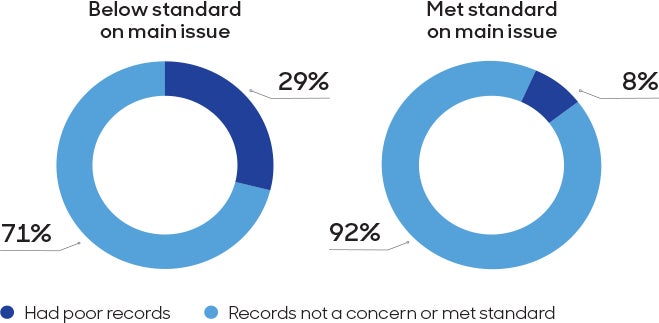
(% of complaints/claims where the assessment of the expected standards on the main factor is known. Cases with 'poor records' are those where the quality of medical records were considered 'below standard'.)
About this analysis
This report is based on our analysis of the underlying themes in nearly 16,000 claims for Avant member doctors from all specialties, including complaints to regulators and compensation claims finalised between 1 July 2019 and 30 June 2024.
Analysis of claims with medical record issues was based on claims and complaints with an issue in the standard of documentation of medical records as the primary or secondary allegation. Medical record issues in claims may be raised by a patient, identified by a regulator or identified by Avant during the claims process.
More information
If you receive a claim or complaint, contact us on 1800 128 268 for expert medico-legal advice- available 24/7 in emergencies.
Avant’s Risk Advisory Service provides personalised support to help proactively reduce your exposure to claims. You can benefit from a personalised risk assessment with a focus on strategy to improve your medical records. Contact us at Risk.Advisory@avant.org.au or visit Risk Advisory Services - Avant.
For any queries on this analysis, please contact us at research@avant.org.au.
Visit our Insights & Resources page for further educational content including webinars, eLearning courses, case studies, articles and factsheets.
IMPORTANT: Avant routinely codes information collected in the course of assisting member doctors in medico-legal matters into a standardised, deidentified dataset. This retrospective analysis was conducted using this dataset. The findings represent the experience of these doctors in the period of time specified, which may not reflect the experience of all doctors in Australia. This publication is not comprehensive and does not constitute legal or medical advice. You should seek legal or other professional advice before relying on any content, and practise proper clinical decision-making with regard to the individual circumstances. Persons implementing any recommendations contained in this publication must exercise their own independent skill or judgement or seek appropriate professional advice relevant to their own particular practice. Compliance with any recommendations will not in any way guarantee discharge of the duty of care owed to patients and others coming into contact with the health professional or practice. Avant is not responsible to you or anyone else for any loss suffered in connection with the use of this information. Information is only current at the date initially published [February 2025].
More ways we can help you



