
6 strategies for effective risk management in an accredited general practice
Running an accredited general practice or specialist clinic comes with many challenges, and managing risks is one of the biggest.
From risks that come with delivering patient care to non-clinical risks posed by the likes of IT systems or regulatory changes, your practice faces a wide range of potential issues.
Even small risks can escalate quickly if not properly managed, and relying on outdated methods can increase the chance of errors.
In this article, we share 6 strategies to help strengthen risk and incident management processes in your accredited general practice or specialist clinic.
1. Identify risks early
A solid risk management strategy starts with identifying not only the clinical risks to your practice, but the non-clinical ones too.
For example, clinical risks might include giving an incorrect vaccination, missing a diagnosis or infection.
An Australian study cited by the RACGP can give you an idea of the occurrence of clinical risks in healthcare practices. The study found that approximately one error occurs for every 1,000 Medicare items billed, and about two errors for every 1,000 patients seen by a GP.
Meanwhile, there are also a range of non-clinical risks accredited general practices and specialist clinics face. These can include the likes of equipment malfunctions, IT system failures, poor cash flow or a shortage of staff.
There are also risks stemming from outside your practice, like changes to legislation, regulations or economic conditions.
A practical example of a non-clinical risk to a healthcare practice is a data breach due to inadequate cybersecurity measures.
For instance, if a practice fails to regularly update its software or implement strong password protocols, hackers could gain access to sensitive patient data.
This could lead to serious legal and financial consequences, such as breaches of privacy laws, fines and loss of patient trust, ultimately damaging the practice’s reputation.
2. Prioritise risks in your accredited general practice
After identifying risks, the next step is to prioritise them based on their likelihood of occurring and potential impact. This allows your accredited general practice or specialist clinic to focus its resources on addressing the most critical risks first.
For example, a high-risk issue like a data breach might require immediate attention, including stronger password policies and encrypted data systems, while lower-risk issues like minor administrative delays may be addressed later.
The RACGP provides an example of a ‘risk matrix’ that can help you classify risks to your practice.
3. Create a robust incident reporting system
Healthcare regulations like the RACGP Standards require accredited general practices to maintain an incident register to record incidents, near misses and corrective actions.
While some practices use spreadsheets or basic documents for this, these outdated methods can make it hard to accurately track risks and incidents, assign tasks or and monitor corrective efforts effectively.
Another solution is to use a digital platform like PracticeHub. Its Quality Registers feature allows you to track risks, incidents and feedback in one place.
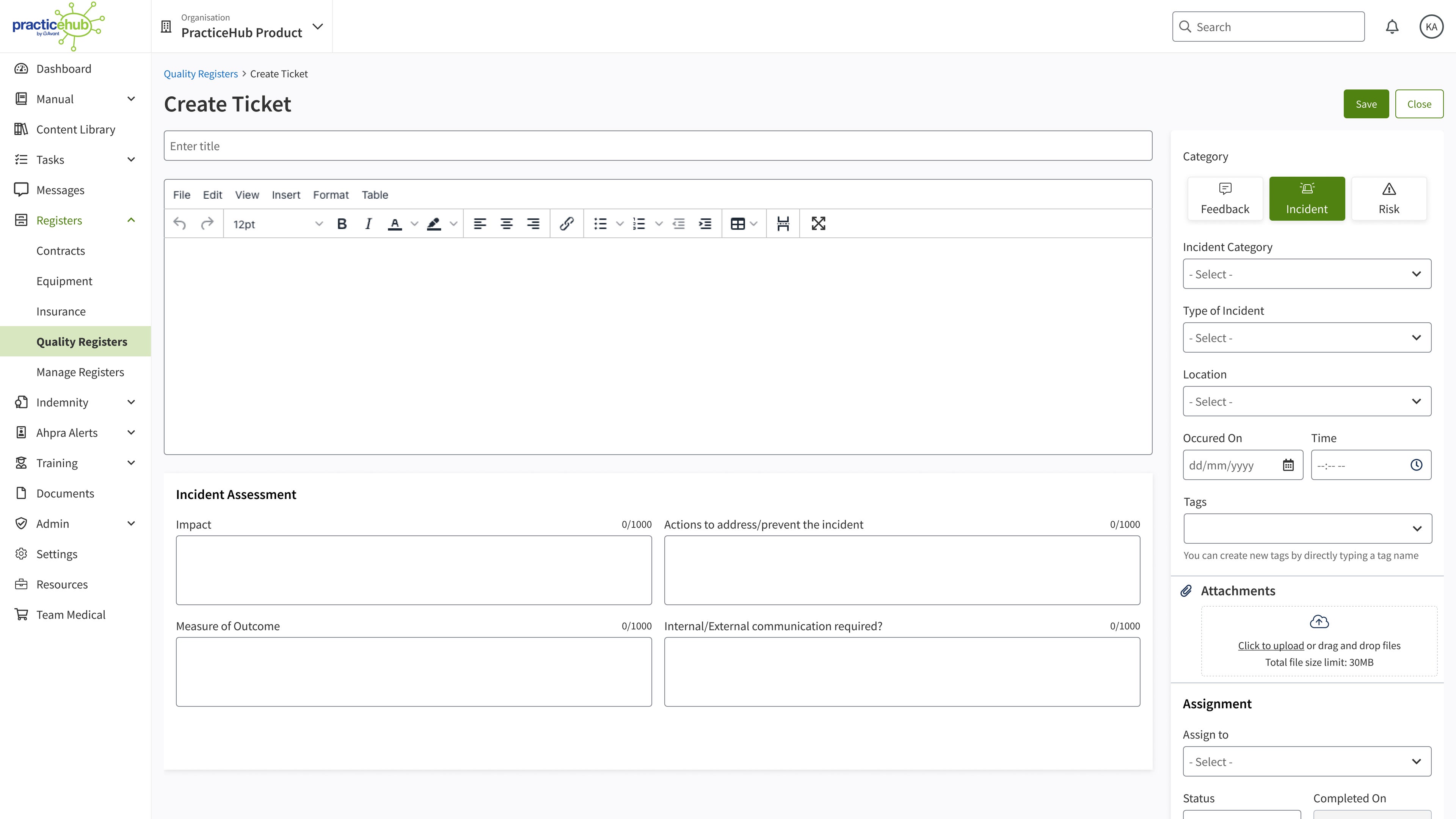
Team members can record incident details in a ‘ticket’ (see the image below) within the platform or via a QR code using their mobile device. You can then easily view the details, assign tasks to staff and monitor their progress via a central dashboard and automatic alerts.
4. Ensure staff receive regular training
Staff training is one of the most important components of effective risk and incident management. Regular training sessions ensure all team members understand their role in maintaining a safe, compliant environment.
This is another area where PracticeHub can help. The platform offers in-built training modules on critical topics like risk management, WH&S, infection control and patient health records, which can help ensure staff are equipped to follow best practice protocols.
5. Foster a culture of safety and transparency in your accredited general practice
Creating a practice culture of safety and transparency, where staff are encouraged to report potential risks without fear of blame, is another best practice approach to risk management.
Managing risk is not only the responsibility of you as the practice manager, but all practice staff. And when staff feel empowered to speak up, it fosters a safer, more transparent environment where risks are addressed promptly.
One way to help create this culture is by including risk awareness in your practice’s mission statement and goals. You could also instil the importance of speaking up about risks via regular emails, posters or by discussing potential risks at team meetings.
6. Conduct regular audits of risk and incident processes
Lastly, ongoing audits are vital to maintaining high standards in an accredited general practice or specialist clinic.
They can help your practice spot gaps in your risk and incident management strategies, ensure risk mitigation efforts are effective and identify new risks.
Free eBook: Incident reporting and risk management simplified
Download our eBook to learn the 5 warning signs that your current risk and incident management system is falling short and how PracticeHub can help you more efficiently manage risks and incidents.
Persons implementing any recommendations contained in this publication must exercise their own independent skill or judgment or seek appropriate professional advice relevant to their own particular practice. Compliance with any recommendations will not in any way guarantee discharge of the duty of care owed to patients and others coming into contact with the health professional or practice. Avant and Avant Practice Solutions are not responsible to you or anyone else for any loss suffered in connection with the use of this information. Information is only current at the date initially published. © Avant Mutual Group Limited 2024.
