How specialist and GP practice management teams can address psychosocial hazards
Thursday, 5 December 2024
Effective specialist and GP practice management requires not only overseeing daily operations but also creating a safe and supportive work environment.
A significant part of this is addressing psychosocial hazards – workplace factors that can harm mental health if not managed.
With recent changes to work health and safety (WH&S) laws, healthcare practices must now take proactive steps to identify and manage these risks.
This article provides an overview of common psychosocial hazards in practices, the requirements under WH&S laws and practical strategies to help safeguard your team.
What psychosocial hazards affect GP practice management teams?
According to Safe Work Australia, a psychosocial hazard is “anything that could cause psychological harm” – meaning factors that negatively impact mental health and well-being.
Common psychosocial hazards in specialist and GP practice management include:
1. High job demands: Staff, including GPs, nurses and admin personnel, often face heavy workloads, leading to stress and burnout.
2. Lack of support: Insufficient managerial or peer support can amplify stress, especially during challenging patient interactions or traumatic events.
3. Role ambiguity: When role expectations aren’t clearly defined, it can lead to confusion, inefficiencies and even legal risks, potentially distressing staff or patients.
4. Poor organisational change management: Abrupt or poorly communicated procedural changes can leave employees feeling undervalued or uncertain.
5. Inadequate recognition: When staff contributions go unnoticed, it can lead to disengagement, affecting morale and productivity.
6. Violence, bullying and harassment: Physical or verbal aggression from patients, or any form of harassment, pose severe psychosocial risks to staff.
What are the legal requirements around psychosocial hazards?
Australian WH&S laws require employers to take proactive steps to manage psychosocial hazards. While requirements across states and territories vary, employers are generally required to:
- Identify psychosocial hazards by observing work conditions, interactions and any situations potentially harmful to mental well-being.
- Assess risks by examining the frequency, duration and severity of exposure to identified hazards.
- Control risks where possible, either by eliminating the hazard or minimising it through workplace policies and supportive resources.
- Review control measures regularly to ensure they remain effective in mitigating risks.
Strategies for addressing psychosocial hazards in GP practice management teams
To help ensure WH&S compliance and support staff well-being, consider implementing the following strategies:
1. Clarify roles and expectations
Imagine this scenario: A receptionist, wanting to help with triage, accesses a patient’s medical record to determine the urgency for a follow-up appointment.
Although well-intentioned, this action is outside of their role and could be a privacy breach.
If discovered, this could cause distress not only for the patient but also for the receptionist, who may have believed they were simply doing a good job.
Role clarity is essential in specialist and GP practice management to prevent such boundary oversteps.
With a digital solution like PracticeHub, you can help ensure your team fully understands their specific roles and responsibilities.
PracticeHub offers customisable position description templates outlining duties and expectations for a variety of practice roles, which you can communicate to all staff within the platform.
2. Develop and maintain policies for psychosocial safety
Consider this common scenario: A staff member frequently dresses outside the prescribed dress code.
Instead of a direct, potentially uncomfortable confrontation, referring them to a dress code policy can depersonalise the discussion, setting expectations in a neutral, professional way.
In specialist and GP practice management, other policies are equally important for preventing psychosocial hazards.
For example, a violence in the workplace policy outlines how to handle confrontational situations, ensuring employees feel safe and supported when interacting with difficult patients.
PracticeHub enables you to store these policies centrally, helping ensure all staff have easy access to review, sign off and reference them as needed. And you don’t need to write them from scratch.
The platform provides over 100 customisable, expertly written policies aligned with RACGP Standards, updated regularly to reflect current WHS laws.
You can assign these policies to team members and track signoffs with instant notifications and a central dashboard (see below).
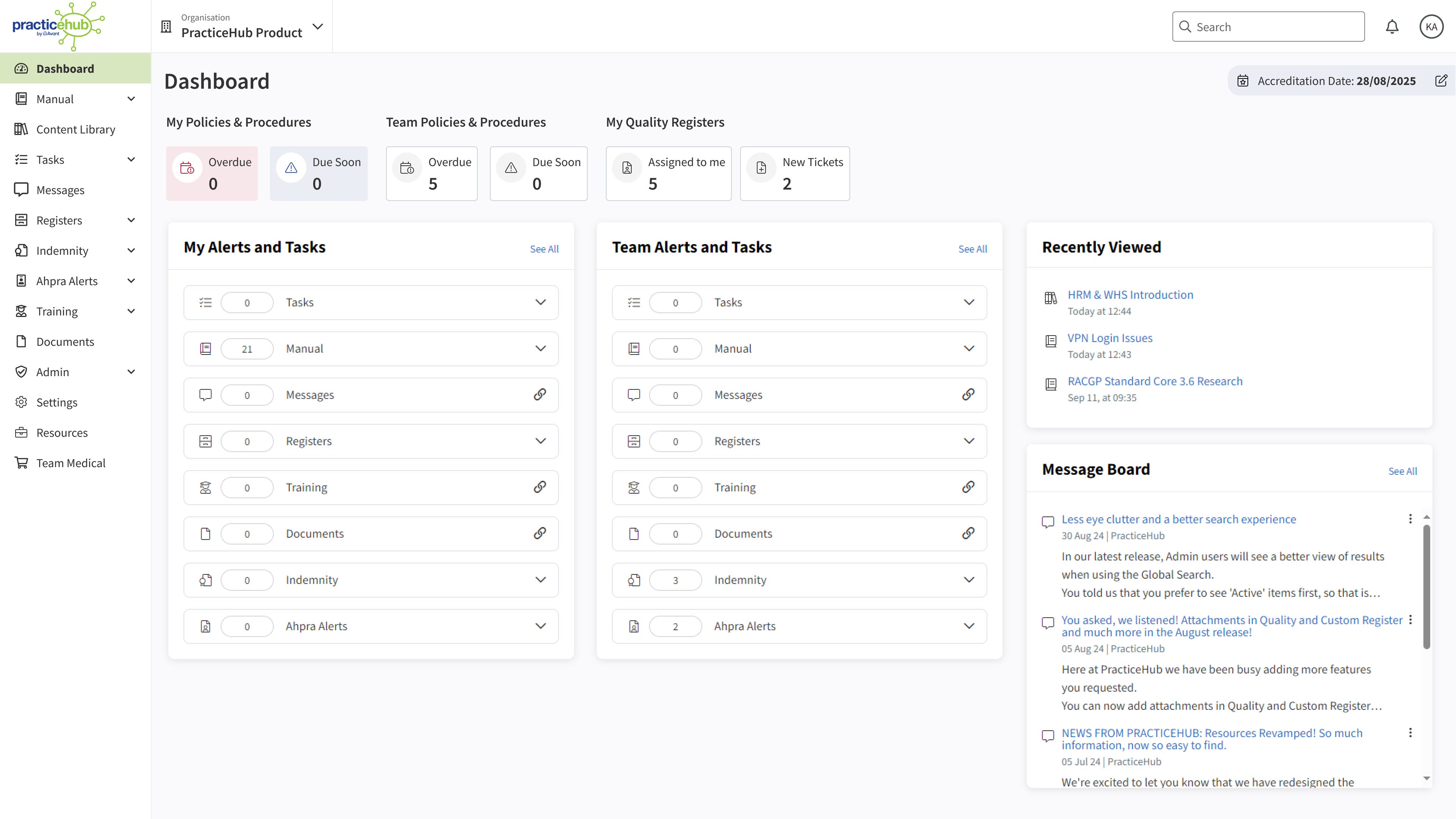
3. Regularly assess and monitor risks
Proactively identifying and assessing psychosocial risks is essential for WH&S compliance, but tracking these risks can be time-consuming – especially when relying on spreadsheets, Word documents and a flood of emails.
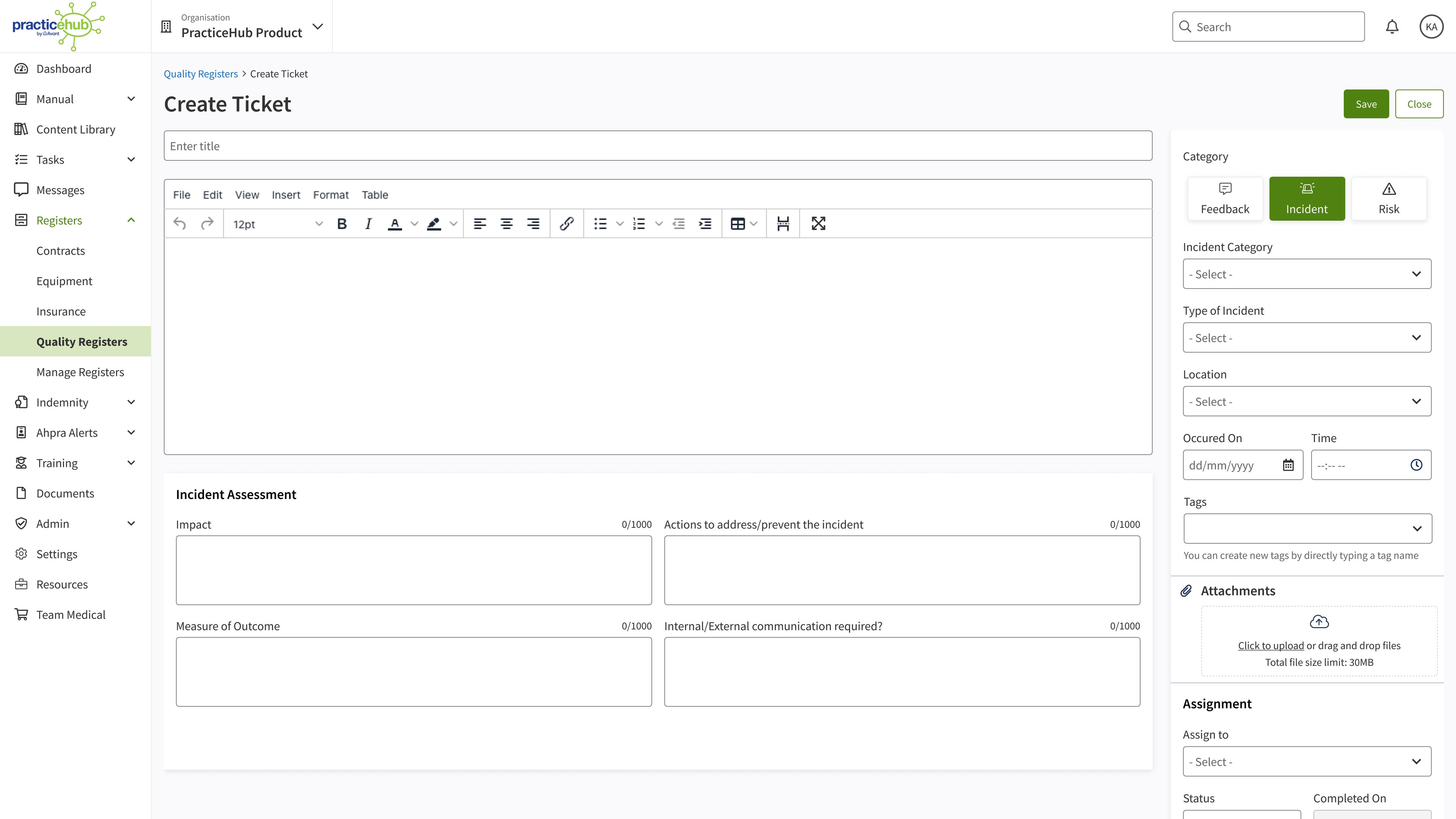
PracticeHub’s Quality Registers module helps streamline this process by providing a central register where you and your team can easily record risks, incidents or feedback.
You can log psychosocial risks in individual “tickets” (see the below image), assign responsibility to a designated staff member for corrective actions and monitor progress through instant alerts and a single dashboard.
This centralised monitoring helps ensure risks are managed effectively, supporting compliance with WH&S and RACGP accreditation requirements.
4. Create a positive, no-blame culture
Creating an environment where staff feel comfortable raising concerns is vital in specialist and GP practice management.
Regularly scheduled meetings, where psychosocial risks are included as agenda items, can reinforce a “see something, say something” culture.
PracticeHub can assist by documenting meeting minutes, recording agreed actions and enabling team members to share their experiences and concerns openly.
5. Protect against psychosocial hazards with online training
Regular training can equip specialist and GP practice management teams with the skills to identify and minimise psychosocial hazards.
While finding time for training can be challenging, PracticeHub helps make it simple. It includes eight e-learning courses on topics like WH&S, patient communication and organisational culture, to help staff prepare for complex or high-stress situations.
For example, the patient communication course can help provide front-office staff with techniques to handle patient complaints in a way that minimises patient anxiety and hostility.
With PracticeHub, staff can complete training at their own pace, whenever is convenient.
See the benefits in action: Book a PracticeHub demo today
Schedule a 30-minute demo with our team today to see how this simple yet powerful platform can help you manage psychosocial risks and simplify everyday practice workflows.
More ways we can help you
Persons implementing any recommendations contained in this publication must exercise their own independent skill or judgment or seek appropriate professional advice relevant to their own particular practice. Compliance with any recommendations will not in any way guarantee discharge of the duty of care owed to patients and others coming into contact with the health professional or practice. Avant and Avant Practice Solutions are not responsible to you or anyone else for any loss suffered in connection with the use of this information. Information is only current at the date initially published. © Avant Mutual Group Limited 2024.



